The governor of Florida, Ron DeSantis was widely quoted last week as saying
“Before COVID did anyone go out and seek testing to determine if they were sick? It’s usually you feel like you’re sick and you get tested to determine what you maybe have come down with.”
As most people will know, the answer is “yes, they did”. You can’t get near a doctor without having your blood pressure measured, because high blood pressure is common, not obvious without testing, and treatable. There are tests performed on infants (for genetic disorders such as PKU and cystic fibrosis), on children (vision and hearing screening), and on the middle-aged and old (cholesterol, glycated hemoglobin, cancer screening). There are tests mainly done for high-risk groups (TB, HIV); there are tests done before you get certain medications (liver or kidney function). Until 1986, Florida required a test to see if you had syphilis in order to get a marriage license. Governor DeSantis has since said that of course he knew all that, and it was obvious he had specifically meant daily or weekly testing for a viral respiratory infection was unprecedented, not all the normal and routine ways people seek out testing to determine if they are sick. And who knows? Maybe he did mean that.
In some ways there’s surprisingly little population screening. Screening has traditionally been popular, because people like knowing things and having explanations. People often argue for more or say they have discovered a way to do more. There are three big barriers in going from a test you take when you feel like you’re sick and one you give to people in advance.
The first barrier is that you have to be able to do something with the result. There’s no point in taking healthy people and finding some illness unless you can do something about it. In the endemic-Covid testing setting, you can isolate and not go infect your workmates or your grandparents or the blokes at the pub or whoever. In the 2004 SARS outbreak we didn’t have rapid antigen tests, but temperature screening was used to find people who might not realise they had SARS or weren’t looking to find out for some other reason.
The second barrier is the base rate problem. The New York Times had a very good story recently about prenatal genetic testing. This looks for very rare genetic disorders, usually as add-ons when testing for Down’s Syndrome. Because those disorders are very rare, most fetuses don’t have them — even most of those who test positive. The Times reported on a set of tests where a positive test had an 80% or higher chance of being wrong. In one sense these tests are very accurate — a negative result is very likely to be correct– but just assuming no-one has these conditions is almost as likely to be correct and has no false positives. The base-rate problem goes together with the problem of what to do; follow-up tests are expensive.
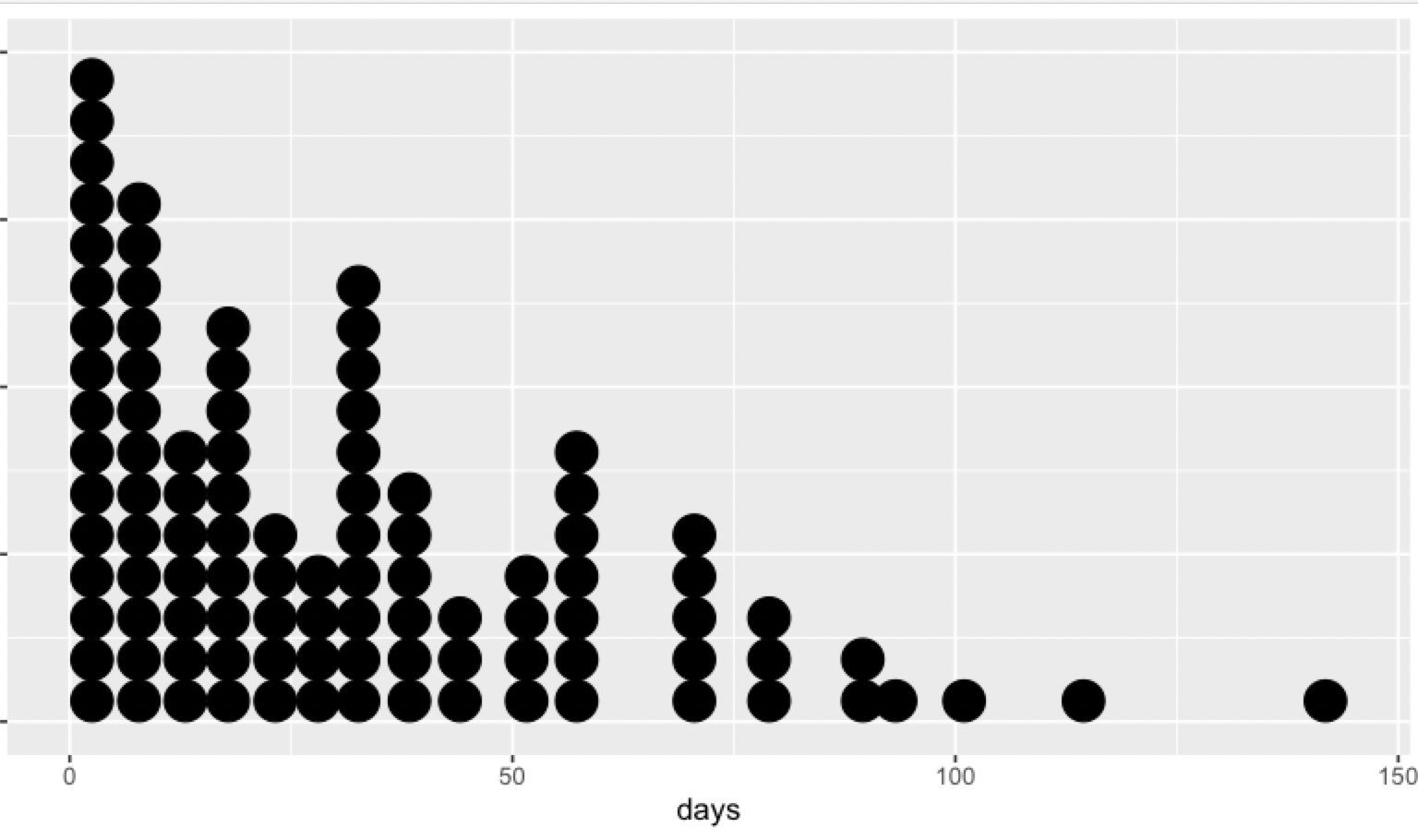
The base rate problem is also an issue for Covid testing here in New Zealand; in contrast to many parts of the world, we currently have very low community prevalence, so a rapid antigen test positive in someone without symptoms or known exposure would very likely be a false positive. In Victoria, the opposite is true: the base rate is high enough that the only rapid antigen tests where PCR follow-up is recommended are those in asymptomatic people with no known exposure.
The third barrier is Rose’s Prevention Paradox: for a lot of diseases, most of the cases don’t happen in high-risk people. There are people at very high risk of heart attack (what Rose was interested in), but they account for a relatively small fraction of all heart attacks. There are people at very high risk of premature birth, but they account for a relatively small fraction of all premature births. Someone with a blood alcohol of 0.2 has a very high risk of getting in a crash, but most car crashes aren’t like that.
Unlike the base-rate problem, Rose’s Prevention Paradox isn’t universal. Testing for the common CFTR mutations will pick up most cases of cystic fibrosis; the Ishihara plates pick up most cases of deficient colour vision; most lung cancer is in smokers; most liver cancer in Western countries is in heavy drinkers or people with Hepatitis B or C.
The Covid example of the prevention paradox is the recent and controversial CDC announcement that most (vaccinated) people who get seriously ill from Covid have co-morbidities. On top of the issue of whether that’s actually a cause for rejoicing, there’s the problem that the majority people who don’t get seriously ill from Covid also have co-morbidities. That is, it’s hard to pick out high risk people. The CDC defined ‘high risk’ very broadly, so that too many people are ‘high risk’; if they define it too narrowly, they would miss a lot of the serious Covid cases.
Very early in the pandemic, the estimate was that a Covid case gave you roughly a year’s worth of mortality risk — if everyone got Covid over a period of one year, death rates for that year would be double what they normally are, across a wide range of subgroups. Omicron is worse than the original strain, but the vaccine helps a lot: vaccinated people are much less likely to die or become hospitalised. Not getting Covid helps even more; masks, ventilation, distancing, testing, etc.